Oral and Maxillofacial Surgery MCQs
MCQs on Local and General Anesthetic Agents – Oral and Maxillofacial Surgery
In this Post you will be able to take quiz containing important MCQs of Oral and Maxillofacial Surgery and topic covered in this Quiz will be Local and General Anesthetic Agents in Oral and Maxillofacial Surgery. Correct Answers are Marked in Bold and Blue colour.
Dental Anesthesia Multiple Choice Questions
- The following are characteristics of the ideal local anesthetic except:
A. Sterilization by autoclave
B. Slow onset
C. Reversible
D. Absence of local reactions - Which portion of the chemical structure of a typical local anesthetic is considered lipophilic (lipid soluble)?
A. Aromatic nucleus
B. Amino group
C. Both a and b
D. Neither a nor b - The mechanism of local anesthetics involves action on:
A. Myelinated nerve
B. Axons
C. Sodium channels
D. Both a and c
E. Both b and c
- Repolarization of a nerve occurs by:
A. Influx of potassium
B. Influx of sodium
C. Efflux of potassium
D. Efflux of calcium
E. None of the above - The following states are characteristics of the salt form of a local anesthetic except one. Which one is the exception?
A. Charged, cation (ionized)
B. Alkaline
C. Crystalline solid
D. Stable - In the presence of an acidic environment, such as infection or inflammation, the amount of free base is reduced; therefore __________ of the local anesthetic is in the ionized form, making anesthesia __________ difficult.
A. More, more
B. More, less
C. Less, more
D. Less, less - The cationic form of a local anesthetic is needed to penetrate the nerve membrane, and the free base form exerts blocking action by binding to the specific receptor site.
A. Both parts of the statement are true.
B. Both parts of the statements are false.
C. The first part of the statement is true, the second part is false.
D. The first part of the statement is false, the second part is true. - Reducing the rate of systemic absorption of a local anesthetic is important when it is used in dentistry because:
A. Otherwise, too large an area would be anesthetized.
B. If not, the anesthesia would not last long enough to complete a dental procedure.
C. The chance of systemic toxicity is reduced.
D. Local anesthesia is associated with respiratory depression. - Addition of vasoconstrictor to local anesthetic:
(1) reduces blood supply to the area,
(2) increases blood supply to the area,
(3) limits systemic absorption,
(4) increases systemic absorption,
(5) reduces systemic toxicity,
(6) increases systemic toxicity.
Which of the three pairs of choices is correct?
A. 1, 3, 5
B. 1, 4, 5
C. 2, 3, 5
D. 2, 3, 6
E. 2, 4, 6 - Local anesthetics cross:
A. The placenta and blood-brain barrier
B. The placenta but not the blood-brain barrier
C. The blood-brain barrier but not the placenta
D. Neither the placenta nor the blood-brain barrier - Which of the following is the preferred local anesthetic technique for hemophiliacs?
A. Nerve block.
B. Supraperiosteal.
C. Intraligamentary.
D. Field block. - Which of the following local anesthetic agent would be preferred in prolonged surgical procedure?
A. Bupivacaine
B. Cocaine
C. Lignocaine
D. Prilocaine - Which of the following is not theory for local anesthetic action?
A. Membrane expansion theory.
B. Calcium displacement theory
C. Electrical potential theory
D. Specific receptor theory
E. None of the above
- Which of the following symptoms is seen in a patient administered with 20-40 % nitrous oxide?
A. Paraesthesia
B. Floating sensation
C. Sweating
D. None of the above - Which of the following about syncope is false?
A. Another term for fainting.
B. Is transient reversible loss of consciousness
C. Caused by altered circulation
D. None of the above
- Which of the following muscles is pierced by the needle while giving an inferior alveolar nerve Block?
A. Medial pterygoid
B. Superior constrictor
C. Temporalis
D. Buccinator
- Which of the following is used to prevent laryngospasm due to GA:
A. Atropine.
B. Epinephrine.
C. Diazepam.
D. Succinylcholine
- Which of the following local anesthetic will be suitable for a hypertensive patient suffering from a heart disease?
A. Lignocaine without adrenaline
B. Prilocaine
C. Lignocaine
D. Lignocaine with adrenaline 1:1000
E. Prilocaine with Felypressin - Which of the following statements regarding the action of local anesthetics is true?
A. More the pH in area less effective is the action of anesthetic agent.
B. Less the pH in area less effective is the action of anesthetic agent.
C. There is little relation between H ion concentration and anesthetic activity
D. There is No correlation between H ion concentration and anesthetic activity - Which of the following is true regarding local anesthetics?
A. They are basic salts of weak acids.
B. Not effective in alkaline pH.
C. Form salts with acids
D. They are acidic salts of weak bases
- In the extraoral technique for mandibular nerve block, the needle after contacting the pterygoid plate is directed:
A. Anteriorly
B. Posteriorly
C. Superiorly
D. Inferiorly - Of the following local anesthetics, which has intrinsic vasoconstrictive action?
A. Cocaine
B. Procaine
C. Xylocaine
D. Bupivacaine - It is difficult to obtain local infiltration anesthesia in the presence of inflammation because of:
A. Decreased pH
B. Increased vascularity
C. Odedma
D. Pain - Alpha adrenergic agonists are used in combination with local anesthetics to:
A. Increase the rate of liver metabolism of local anesthetic
B. Increase the concentration of LA at receptor site
C. Stimulate myocardial contraction
D. Increases vascular absorption of LA - Action of toxic doses of local anesthetic on CNS can be described as:
A. First stimulating the CNS followed by depression
B. First depressing it followed by stimulation
C. Only depression of the CNS
D. Only stimulation of the CNS - To give field block, the LA should be deposited near:
A. Main trunk
B. Large branch of peripheral nerve
C. Small nerve endings
D. Periodontal ligament - Most accepted theory for conduction of pain is:
A. Gate control theory
B. Specificity theory
C. Membrane stabilization theory
D. None of the above - In anesthetizing lower anteriors, all of the following are indicated except:
A. Fischer 123 technique
B. Classical inferior alveolar nerve block
C. Mental nerve block
D. Incisive block - Action of lignocaine is affected by all except:
A. PH at the site of injection
B. Blood flow at the site of injection
C. Vasoconstrictor in the LA solution
D. Action of cholinesterase at the site of injection
- The addition of hyaluronidase to a local anesthetic solution might:
A. Increase the duration of anesthesia
B. Limit the area of anesthesia
C. Reduce bleeding
D. Enhance diffusion of local anestheticTemporomandibular joint (TMJ) MCQs
- The effect of local anesthesia can be increased by the addition of:
A. Adrenaline
B. Isoprenaline
C. Dopamine
D. Felypressin (synthetic vasopressin) - Amide type of local anesthetic agents undergo biotransformation primarily in the:
A. Kidney
B. Liver
C. Plasma
D. Excreted in the unaltered form - The maximum dose of lignocaine without adrenaline that can be admitted to a patient is:
A. 4 mg/kg body weight
B. 5 mg/kg body weight
C. 7 mg/kg body weight
D. 9 mg/kg body weight - Surgery is carried out in which stage of general anesthesia?
A. Plane I
B. Plane II
C. Plane III
D. Plane IV - The amount of vasoconstrictor in 1 ml of 2 % lignocaine solution with 1:200000 adrenaline is:
A. 0.5 mg
B. 0.05 mg
C. 0.005 mg
D. 0.0005 mg - Inferior alveolar nerve block alone can be used in:
A. Pulpotomy of third molar
B. Apicoectomy of third molar
C. Extraction of first molar
D. Root resection of first molar - A bilateral mandibular block
A. Is dangerous because patient may swallow tongue
B. Will lead to space infection
C. Is not contraindicated
D. Should rarely be performed - Which of the following general anesthetic techniques should be used for anesthesia in oral surgery?
A. Open drop method
B. Anesthesia with nasopharyngeal airway
C. Nasoendotracheal tube with throat pack
D. IV anesthesia with nitrous oxide and oxygen - The longest acting, most potent and most toxic LA is:
A. Lidocaine
B. Dibucaine
C. Bupivacaine
D. Tetracaine - For extraction of mandibular molar, anesthesia is given to act on:
A. Inferior alveolar nerve
B. Buccal nerve
C. Lingual nerve
D. Masseteric nerve - Among the following, which condition is a contraindication to the use of local anesthetic agent?
A. Parkinson’s disease
B. Liver damage
C. Pregnancy (third trimester)
D. Hypersensitivity to the drug
- Inferior alveolar nerve block is absolutely contraindicated in patients suffering from the following disease:
A. Thrombocytopenia
B. Hemophilia
C. Hypoprothrombinemia
D. von Willebrand’s disease - Myelinated nerve fibers have all of the following properties except:
A. Conduction is slower in myelinated than in non myelinated fibers
B. Current discharges at nodes of Ranvier
C. Outer layer is of lipids
D. Depolarisation occurs only at nodes of Ranvier - Each of the following side effects can occur as a result of systemic absorption of lidocaine except one. Which is the exception?
A. Increased gastric motility
B. Tonic clonic convulsions
C. Decreased cardiac output
D. Repiratory depression - Lidocaine is used more commonly in dentistry because lidocaine:
A. Causes less depression of the CNS
B. Causes less cardiovascular collapse
C. Causes lesser incidence of allergic reactions
D. Is 50 times more potent than procaine - Of the following, in which condition local anesthesia is ineffective?
A. Edema
B. Localized infection
C. Hematoma
D. Anemia - LA with adrenaline is absolutely contraindicated in:
A. First trimester of pregnancy
B. Hyperthyroidism
C. Hemophilia
D. Hypertension - In systemic LA toxicity, there is:
A. Post depression convulsion
B. Post convulsion depression
C. Convulsions
D. Depression - Which of the following local anesthetic will be suitable for a hypertensive patient suffering from a heart disease?
A. Lignocaine without adrenaline
B. Prilocaine
C. Lignocaine with adrenaline 1:1000
D. Prilocaine with Felypressin - Maximum dose of xylocaine without adrenaline that can be given in a 60 kg adult is:
A. 500 mg
B. 300 mg
C. 400 mg
D. 600 mg - When blocking a nerve containing both motor and sensory fibers, the last functional property lost is:
A. Temperature
B. Pain
C. Proprioception
D. Touch - Most difficult maxillary tooth to anesthetize by infiltration is:
A. First molar
B. First premolar
C. Canine
D. Third molar - In case of Gow-Gates technique , the target area is:
A. Neck of condyle
B. Head of the condyle
C. Medial side of the ramus
D. Lateral side of the condyle - Improper direction of the needle insertion during inferior alveolar nerve block results in:
A. Facial nerve paralysis
B. Paraesthesia
C. Hematoma
D. Trismus - The closed mouth technique for mandibular nerve block is:
A. Clark and Holmes technique
B. Akinosi, Vazirani technique
C. Gow Gates technique
D. Angello sergenti technique - Hematoma formation is more frequent with:
A. Inferior alveolar nerve block
B. Posterior superior alveolar nerve block
C. Greater palatine nerve block
D. Infraorbital nerve block - Toxicity of local anesthesia is reversed by:
A. IV epinephrine
B. IV nalorphine
C. IV barbiturates
D. IV sodium bicarbonate - How much lignocaine is present in 2.0 ml of 2% lignocaine solution ?
A. 40 mg
B. 20 mg
C. 30 mg
D. 2 mg - Sensitivity to local anesthetics is greater in:
A. Type B fibers
B. Type C fibers
C. Type A delta fibers
D. Fibers supplying the muscle spindles - A patient manifests systemic symptoms of pallor and unconscious following local anesthesia. The patient is experiencing:
A. CNS depression
B. Syncope
C. Tonic reaction to local anesthesia
D. Allergic response - Which of the following can be used as a local anesthetic agent if a patient is allergic to amide and ester anesthetic derivatives?
A. Nitrous oxide
B. Bupivacain
C. Phenylephrine
D. Diphenhydramine
- Each of the following statements about local anesthesia is correct except:
A. Lignocaine causes cardiac dysarrhythmia
B. Prilocaine is more toxic than lignocain
C. Prilocaine and lignocaine are the components of EMLA (eutectic mixture of local anesthetics)
D. Bupivacaine is given for obstetric epidural anesthesia - The local anesthetic which has sympathomimetic property is:
A. Procaine
B. Lidocaine
C. Cocaine
D. Tetracaine - Which of the following respiratory conditions is most alarming during patient sedation in dental clinic:
A. Apnea
B. Dyspnea
C. Hyperapnea
D. Tachypnea - The onset of action of lidocaine is after:
A. 1-2 minutes
B. 5-10 minutes
C. 3-5 minutes
D. 7-8 minutes - In dentistry which sedatives are generally used?
A. Benzodiazepines
B. Morphine
C. NSAID
D. Pethidine - A patient who faints during extraction should be positioned in the:
A. Lateral position
B. Horizontal position
C. Trendelenburg position
D. Dorsosacral position - The action of adrenaline is potentiated in the presence of all except:
A. Halothane
B. Ethyl chloride
C. Cyclopropane
D. Ether
- Syncope:
A. Is associated with bradycardia and loss of consciousness
B. Never occurs in children
C. Always associated with hypoglycemia
D. Best treated in a sitting posture - The dose of epinephrine given in anaphylaxis:
A. 0.5 mg in 1:1000 IM
B. 0.5 mg in 1:10000 IM
C. 0.5 mg in 1:500 IM
D. 1 mg in 1:100 IM - LA acts on nerve membrane by:
A. Blocking conductance of Na+ from interior to exterior
B. Blocking conductance of Na+ from exterior to interior
C. Blocking conductance of K+ from exterior to interior
D. Blocking conductance of K+ from interior to exterior - On administration of LA in an area of infection, it is not effective because of the increase in:
A. Cations
B. Free base
C. Uncharged base
D. None - The common complication of the local anesthetic prilocaine is:
A. Agranulocytosis
B. Hepatic dysfunction
C. Methemoglobinemia
D. Loss of taste - The action of long acting muscle relaxants used during GA may be terminated by:
A. Neostigmine
B. Atropine
C. Ketamine
D. Succinylcholine - Rapid onset of action seen by local anesthesia in small nerve endings is due to:
A. Increased threshold of small nerves due to depolarization
B. Low pH of small nerve fibers
C. High ratio of surface area to the volume of small nerve fibers
D. Increased resting potential of small nerve fibers - The cause of sensation of tissue tearing during local anesthesia administration is due to:
A. Passage through a cyst
B. Passage through a muscle
C. Passage through an area of infection
D. Barb on the needle
- Increased incidence of reaction to LA will occur by:
A. Rapid rate of injection
B. Using an aspirating technique
C. Addition of vasoconstrictor to the solution
D. Premedication with barbiturate - Which of the following local anesthetic is a vasoconstrictor:
A. Lidocaine
B. Procaine
C. Bupivacaine
D. Ropivacaine
- Excess of plasma level of lignocaine can cause cardiovascular collapse due to:
A. Myocardial depression
B. Vagal stimulation
C. Syncope
D. CNS excitability - Syncope is usually caused by:
A. Vasoconstriction
B. Cerebral ischemia
C. Cerebral hyperemia
D. Decrease in the vascular bed - First local anesthetic to be used clinically was:
A. Cocaine
B. Bupivacaine
C. Procaine
D. Lignocaine - Which of the following inducing agents has analgesic property?
A. Nitrous oxide
B. Halothane
C. Enflurane
D. Sevoflurane - Maximum recommended dose of lignocaine with epinephrine is:
A. 5mg/kg body weight
B. 7 mg/kg body weight
C. 10 mg/kg body weight
D. 15 mg/kg body weight - The most common anesthetic complication occurring within first 24 hours after surgery under general anesthesia is :
A. Hypertension
B. Renal failure
C. Atelectasis
D. Cardiac arrest - The activity of procaine is terminated by:
A. Elimination by kidney
B. Storage in the adipose tissue
C. Metabolism in the liver only
D. Metabolism in the liver and by pseudocholinesterase in the plasma
- Xylocaine strength used in dentistry is:
A. 2 %
B. 5 %
C. 8 %
D. 10 % - The most significant adverse consequence of accidental intravenous administration of local anesthetic is:
A. Bronchoconstriction
B. Hepatic damage
C. Nerve damage
D. Seizures
- The first sensation to be lost following administration of local anesthetic is:
A. Proprioception
B. Pain
C. Touch
D. Temperature - Most commonly used local anesthetic:
A. 1:20000 xylocaine HCl
B. 1:50000 xylocaine HCl
C. 1:10000 xylocaine HCl
D. 1:80000 xylocaine HCl - The safe dose of adrenaline in a patient with compromised cardiac condition is:
A. 0.2 mg
B. 0.02 mg
C. 0.4 mg
D. 0.04 mg
- Cartridges shouldn’t be permitted to soak in alcohol because it:
A. Destroys vasoconstrictor
B. Is less effective
C. Is warm in sensation
D. Diffuses through rubber cap causing contamination
- Sedation by which the following routes can be reversed most rapidly?
A. Oral
B. Inhalation
C. Intravenous
D. Intramuscular - With over dosage of LA agent, one would observe:
A. Hypertension
B. Hypotension
C. No change in BP
D. Cardiac arrhythmias - The role of sodium metabisulphite in local anesthetic agent is:
A. Preservative
B. Fungicide
C. Reducing agent
D. Vasoconstrictor - Symptoms of epinephrine overdose following a local anesthetic injection may include all of the following except:
A. Restlessness
B. Hypotension
C. Apprehension
D.Palpitations - Trismus during block anesthesia is as a result of:
A. Massive edema
B. Damage to medial pterygoid
C. Damage to lateral pterygoid
D. Damage to inferior alveolar nerve - Allergic reactions in patients who receive amide type local anesthetics for dental procedures are most likely caused by the reaction of:
A. Methylparaben
B. Contaminants
C.Lignocaine hydrochloride
D. Epinephrine - ECG changes can first be observed when level of lignocaine is more than:
A. 5-6 mcg/ml
B. 10-12 mcg/ml
C. 2-4 mcg/ml
D. 1.2 mcg/ml - Inferior alveolar nerve block is given in:
A. Retromolar area
B. Pterygomandibular space
C. Submandibular space
D. Submental space - The color of a nitrous oxide cylinder is:
A. Red
B. Blue
C. White
D. Black - Which of the following is not used as a topical LA?
A. Procaine
B. Tetracaine
C. Lidocaine
D. Benzocaine - Local anesthetic is not effective in an inflamed tissue because:
A. All impulses generated cannot be blocked
B. Myelin sheath is inflamed so it does not absorb the solution
C. pH is more acidic, so LA is ineffective
D. All of the above - The earliest sign of syncope is:
A. Pallor
B. Constriction of pupil
C. Dilatation of pupil
D. Bradycardia - For extraoral maxillary nerve block, the target area is:
A. Anterior to lateral pterygoid plate
B. Posterior to lateral pterygoid plate
C. Pterygomandibular fossa
D. Pterygomandibular fissure - The primary excretory organ for the local anesthetic and its metabolites is:
A. Lungs
B. Kidneys
C. Rectum
D. Skin - Maximum allowable dose of 2% lidocaine with 1:100000 epinephrine for a child of 40 lbs is:
A. 60 mg
B. 120 mg
C. 180 mg
D. 240 mg - Which combination forms day care anesthesia?
A. Fentanyl, propofol, isoflurane
B. Pethidine, propofol, isoflurane
C. Thiopental, pethidine, halothane
D. Thiopental, isoflurane, fentanyl - “Kelsey Fry Technique” refers to the removal of:
A. Impacted maxillary third molars
B. Impacted mandibular third molars
C. Impacted mandibular canines
D. Impacted maxillary canines - Sodium bicarbonate when given with local anesthetics has which of the following effect?
A. Increases speed and quality of anesthesia
B. Decreases diffusion of the anesthetic drug
C. Causes rapid elimination of the local anesthetic
D. Decreases speed and quality of anesthesia - Nerves anesthetized in incisive nerve block are
A. Incisive nerve only
B. Incisive and mental nerve
C. Incisive and inferior alveolar nerve
D. Mental and inferior alveolar nerve - A patient presents with trismus. Which of the following technique will block mylohyoid nerve, incisive, and long buccal nerve?
A. Akinosi’s technique
B. Gow Gate’s technique
C. V block technique
D. Conventional inferior alveolar nerve block - Pterygomandibular space contains all except:
A. Nerve to mylohyoid muscle
B. Long buccal nerve
C. Loose areolar tissue
D. Nerve to medial pterygoid muscle - Which one of the following local anesthetics belongs to the ester group?
A. Procaine
B. Bupivacaine
C. Lignocaine
D. Mepivacaine - All of the following are complications of LA toxicity except:
A. Cardiac depression
B. CNS depression
C. Paresthesia
D. Respiratory depression - Which of the following intravenous induction agents is most suitable for day care surgery?
A. Morphine
B. Ketamine
C. Propofol
D. Diazepam - An anesthetist orders a new attendant to bring the oxygen cylinder. He should order to bring:
A. Black cylinder with white shoulder
B. Black cylinder with grey shoulder
C. White cylinder with black shoulder
D. Grey cylinder with white shoulder - The agent of choice to reverse status epilepticus inducted by local anesthetic overdose is:
A. Oxygen
B. Diazepam
C. Epinephrine
D. Phenobrbital - Toxic effect of local anesthetic include:
A. Convulsions
B. Asystole
C. Methemoglobinemia
D. All of the above
- All of the following drugs are used for anesthetic emergencies EXCEPT:
A. Aminophylline
B. Epinephrine
C. Atropine sulfate
D. Amoxycillin
- The anatomical landmark used during posterior superior alveolar nerve block are mucobuccal fold, occlusal plane, coronoid process and:
A. Anterior border of ramus
B. Mandible
C. First premolar
D. Midline - During mandibular nerve block, which nerve might also get damaged?
A. Abducent
B. Facial
C. Vagus
D. Trochlear - The sudden appearance of dumbell shaped swelling during third molar nerve block is mainly due to:
A. Injection in pterygoid plexus
B. Injection in parotid gland
C. Injection into internal maxillary artery
D. Injection into nasal cavity - The maximum concentration of lidocaine for topical block is
A. 2 %
B. 4 %
C. 15 %
D. 10 % - Which of the following are the theories of regional anesthesia?
A. Specificity theory and gate control theory
B. Specific receptor theory and gate control theory
C. Specific receptor theory and membrane expansion theory
D. Specificity theory and membrane expansion theory - The maximum dose of LA must be reduced when used in combination with a CNS/respiratory depressant because, it may result in:
A. Seizures
B. Coma
C. Death
D. All of the above
- Bupivacaine, a local anesthetic agent, is used in dentistry in the concentration of:
A. 2 %
B. 4 %
C. 5 %
D. 0.5 %
- The site of action of local anesthetic is on:
A. Axioplasm
B. Epineurium
C. Nerve membrane
D. Perineurium - True regarding EMLA is:
A. It is a mixture of 24 mg/g Lidocaine and 25 mg/gm prilocaine used for skin anesthesia
B. Used as general anesthetic in pediatric use
C. Used for bilateral nerve block
D. All of the above - The gas used in LA cartridge is:
A. Oxygen
B. Helium
C. Nitrogen
D. Carbondioxide - A painless, fluid filled retention cyst appearing in the area of recent dental treatment may be the result of:
A. Failure of absorption of the anesthetic
B. Allergic reaction of agents employed
C. Injection occurred during treatment
D. Injury to salivary gland
- Which of the following local anesthetic is active topically?
A. Lidocaine and Benzocaine
B. Lidocaine and Mepivacaine
C. Mepivacaine and Benzocaine
D. Prilocaine and Mepivacaine - Eutectic mixture of 2.5 % lignocaine and 2.5 % prilocaine is used for:
A. Gow Gate’s technique for mandibular nerve block
B. Gasserian ganglion block
C. Intrapulpal anesthesia
D. Anesthetizing intact mucosa
- The most common emergency seen after the use of local anesthetic is
A. Trismus
B. Toxic reaction
C. Swelling
D. Syncope
- In CPR, the sternum should be depressed at the rate of:
A. 1 inch per second
B. 2 inch per secon
C. 1 inch per 5 second
D. 2 inch per 5 second - Properties of local anesthetic include all of the following EXCEPT:
A. Preferentially bind to sodium channels in open and inactivated state
B. Low affinity for channels in resting state
C. They are weak bases
D. Less effective in an environment with low extracellular pH - Nitrous oxide alone is not used as a GA agent because of:
A. Difficulty in maintaining an adequate oxygen concentration
B. Expense of the agent and its exposure hazards
C. Adverse effect on liver
D. Poor analgesic property - Fibers which transmit fast pain from pulp are:
A. A alpha
B. A beta
C. A gamma
D. A delta
- In posterior superior alveolar nerve block, the needle is advanced in an:
A. Upward, outward and forward direction
B. Upward, inward and backward direction
C. Upward, outward and backward direction
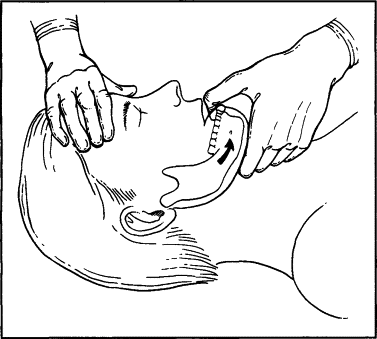
D. Downward, inward and forward direction - The head tilt procedure while dealing with an unconscious patient in dental chair is done to ensure:
A. Patent airway
B. Blood circulation to the brain
C. To clear the foreign body obstacle
D. To relieve spasm of repiratory muscles - For Propofol all are true EXCEPT:
A. Has a rapid recovery rate
B. Used for induction and maintenance of anesthesia
C. Causes vomiting after use
D. Causes sedation - Which among the following should be the last resort for giving LA technique to the patient?
A. Intrapulpal
B. Intraligamentary
C. Intraosseous
D. Infiltration - When soft palate is paralysed, which is not seen?
A. Clefting of the palate
B. Nasal regurgitation
C. Nasal twang
D. Flat palate - The potential action of all the local anesthetics depends upon the ability of anesthetic salt to liberate the free:
A. Acid medium
B. Neutral medium
C. Alkaloidal medium
D. Alkaloidal base
- Local anesthetics block nerve conduction by:
A. Depolarising the nerve membrane reducing threshold potential
B. Decreasing the membrane permeability to Na+ ions thereby stabilizing nerve membrane
C. Increasing the membrane permeability to K+ ions and by depolarising the nerve membrane
D. None of the above - Anterior trunk of mandibular branch of trigeminal nerve supply all EXCEPT:
A. Medial pterygoid
B. Lateral pterygoid
C. Masseter
D. Temporalis - Gate control theory of pain is due to:
A. Substantia gelatinosa
B. A delta fibers
C. C- fibers”
D. Free nerve endings - Infraorbital anesthesia involves which nerve?
A. Anterior superior alveolar nerve
B. Posterior superior alveolar nerve
C. Facial nerve
D. Mandibular nerve - Objective signs of inferior alveolar nerve block are seen in:
A. Unilateral midline between premolars and incisors
B. Bilaterally between premolars and incisors
C. Unilateral midline between second molar and incisor
D. Bilateral midline between second molar and incisor - A ligamental injection of 2 % lidocaine with 1:10000 epinephrine will cause the pulp circulation to:
A. Cease for about 30 minutes
B. Remain the same
C. Increase markedly
D. Decrease slightly - Local anesthetic with lowest placental transfer rate is:
A. Lignocaine
B. Bupivacaine
C. Mepivacaine
D. Chloroprocaine
- If injection of LA with adrenaline goes into vessel accidentally, what will happen?
A. Hypotension + Bradycardia
B. Hypertension + Bradycardia
C. Hypertension + Tachycardia
D. Hypotension + Tachycardia - A patient who had a history of hepatitis one month ago should be preferably given which anesthetic agent?
A. Lignocaine
B. Bupivacaine
C. Procaine
D. Procainamide - One of the disadvantages of breech loading, metallic type, self aspirating, cartridge type syringe is:
A. Autoclavable
B. Rust resistant
C. Piston is scored
D. Weight
- Which of the following technique of local anesthesia requires extraoral landmarks?
A. High tuberosity approach
B. Fischer 123
C. Gow Gates
D. Vazirani Akinosi - Which is the extraoral landmark for Gow Gates technique of mandibular nerve block?
A. Corner of the mouth
B. Intertragic notch
C. Both of the above
D. None of the above - All are true about use of articaine in a child except:
A. Its an amide which is metabolized in liver
B. Plasma half life is 90 minutes
C. Infiltration produces adequate anesthesia in primary molar so need for block anesthesia is eliminated
D. More breakdown cause less toxicity - Which preservative is most commoly used in LA in India?
A. Methyl hydroxyl benzoate
B. Cetrimide
C. Sodium Paraben
D. Silica gel - Which of these is pierced during posterior superior alveolar nerve block?
A. Medial pterygoid
B. Lateral pterygoid
C. Buccinator
D. Masseter - Most potent topical anesthetic is:
A. Mepivacaine
B. Prilocaine
C. Benzocaine
D. Tetracain
- Maximum permissible dose of articaine in a healthy patient is:
A. 1.3 mg/kg
B. 5 mg/kg
C. 2 mg/kg
D. 7 mg/kg
- LA is deposited in inferior alveolar nerve block at:
A. Sigmoid notch
B. Coronoid notch
C. Lingula
D. Groove of mandibular neck - The following affects the duration of local anesthesia EXCEPT:
A. Protein binding capacity of local anesthetic
B. Addition of vasoconstrictor
C. Vasodilator activity of local anesthetic
D. Non-nervous tissue diffusibility
- Local anesthetic with highest local tissue irritancy is:
A. Procaine
B. Chloroprocaine
C. Lignocaine
D. Bupivacaine
- Which space has highest chance of infection with the injection of classical inferior alveolar nerve block?
A. Lateral pharyngeal space
B. Pterygomandibular space
C. Parapharyngeal space
D. Pretracheal space - Which of the following statements is TRUE of local anesthesia?
A. Local anesthesia eliminates the feeling of sensation without the loss of consciousness.
B. Local anesthesia is an unpleasant sensory and emotional experience.
C. Local anesthesia eliminates the feeling of sensation through loss of consciousness.
D. Local anesthesia is never necessary for dental hygiene appointments - The first local anesthetic was:
A. lidocaine.
B. Cocaine.
C. Novocaine.
D. Articaine. - Which of the following defines pain threshold?
A. A neurologic experience of pain
B. The personal interpretation and response to the pain message
C. The point at which a sensation becomes painful, resulting in discomfort
D. A method or tool used to measure pain